Get Healthy!
- Posted February 6, 2026
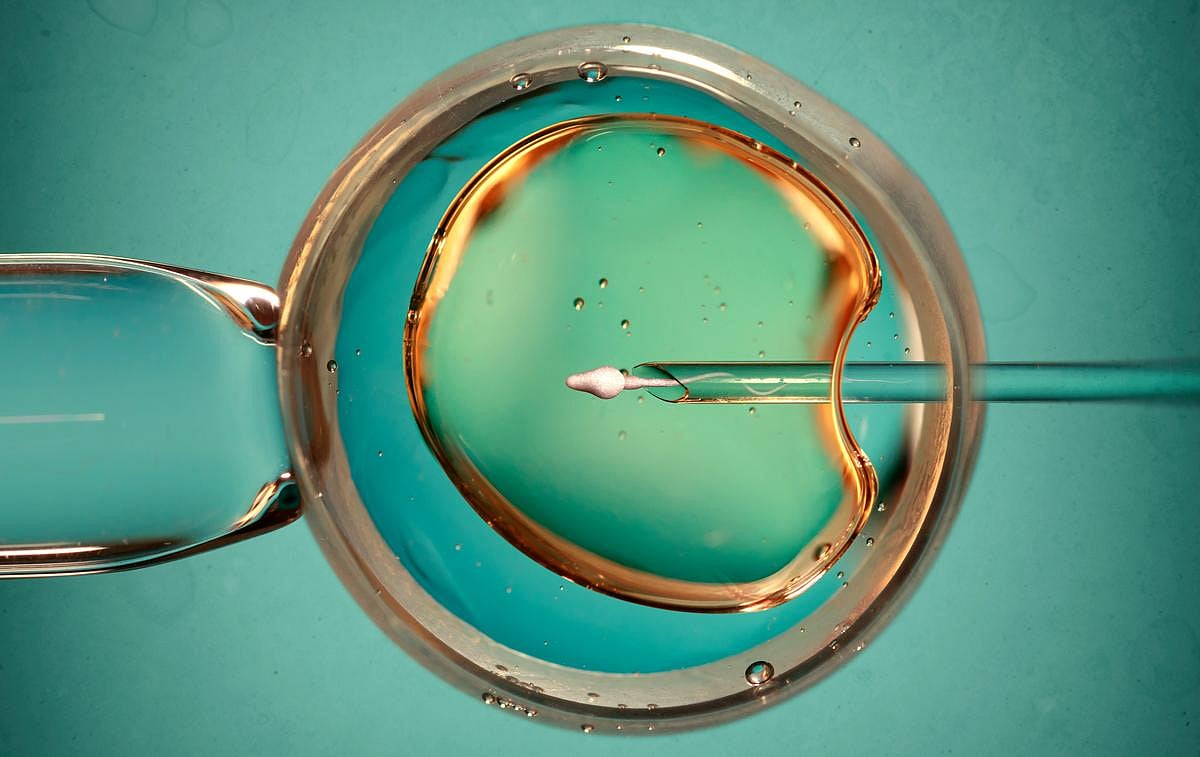
A 'Natural' Option For IVF Is As Effective In Producing Healthy Babies, Trial Shows
A slightly more complicated method of in vitro fertilization (IVF) might produce better results for mother and baby, a new Chinese clinical trial has found.
Timing implantation of a frozen embryo to a woman’s natural ovulation cycle is as effective at achieving a healthy baby as current standard IVF, which involves using hormone treatment to “program” a woman’s ovulation, researchers recently reported in The BMJ.
Importantly, implanting a frozen embryo during natural ovulation came with less risk of pregnancy complications like pre-eclampsia, the trial showed.
“A natural ovulation regimen was as effective as a programmed regimen for achieving a healthy live birth, but with a lower rate of pre-eclampsia,” concluded the research team led by Dr. Zi-Jiang Chen, a professor of obstetrics and gynecology at Shandong University in China.
“Birth weight and the risks of neonatal complications did not differ between the two regimens,” the researchers added.
The Chinese study has produced results in advance of a U.S. clinical trial that's examining the same question, said Dr. Anne Steiner, president of the Society for Reproductive Endocrinology and Infertility.
If the U.S. trial offers similar results, it could change the way many IVF procedures are performed, Steiner said.
“If we see the same kind of results from the American trial, then I certainly could see that the default would be for natural ovulation, and then programmed ovulation would be reserved for certain circumstances,” she said.
About 60% of IVF procedures currently involve transplant of a frozen embryo, researchers said in background notes.
However, there’s been “longstanding controversy” over whether hormone-driven ovulation is better than natural ovulation for achieving a live birth, researchers said.
“The standard for a long time has been what we call programmed cycle, where you give a woman a little bit of estrogen for two weeks and then add some progesterone, some hormones, and then you do the embryo transfer,” Steiner said.
“This allows the embryo transfer to be scheduled, and it's a little bit easier on couples because they know exactly the date and it can be all scheduled out and easy,” she said.
However, IVF with a frozen embryo also can be timed to a woman’s natural ovulation, Steiner said.
“There are hormonal changes that occur at the time of ovulation such that you could transfer the embryo into the uterus when a normal embryo would be entering the uterus,” Steiner said.
This timing requires more work, she said.
“Timed with her ovulation, there can be more visits. They don't know when the transfer is going to fall, because ovulation doesn't always occur on the same day, and so a woman has to be monitored,” Steiner added. “There's a little bit more monitoring and oversight, and the woman still takes hormones — it's just less hormones.”
However, early data had suggested that there might be fewer pregnancy complications through natural ovulation versus programmed ovulation, researchers said.
For the Chinese trial, researchers recruited nearly 4,400 women at 24 fertility centers in China who were about to undergo IVF through frozen embryo transfer.
Half of the women were randomly chosen to have IVF based on natural ovulation, while the other half had the embryo planted on standard programmed ovulation.
About the same percentage of women had a healthy live birth in either group, the study found – 42% in natural ovulation and 41% in the programmed regimen.
However, the trial also found that the risk of pre-eclampsia was significantly lower in the natural ovulation group, 2.9% versus 4.6%.
The natural ovulation group also had lower rates of:
Early pregnancy loss (12% versus 15%)
Placental accreta spectrum, when the placenta fails to detach easily after birth (2% versus 4%)
Caesarean section (70% versus 76%)
Postpartum hemorrhage, or severe bleeding after childbirth (2% versus 6%)
“One thing that's really encouraging and potentially of note and importance is that they did have lower preeclampsia and pregnancy complications in the group that timed with natural ovulation,” Steiner explained.
But even if the U.S. trial confirms these findings, it’s likely that both methods will continue to be offered to women going through IVF, she added.
“Not everybody can use the natural ovulation method, and we don’t ever want to take options away because we want flexibility,” Steiner said. “It may be that it’s just too difficult to time with ovulation, and it can be easier to do medicated cycles for people.”
Bottom line?
“Basically, the take home point is that both are good options for preparing the uterus,” Steiner concluded. “They’re both equally effective.”
More information
The American Pregnancy Association has more on in vitro fertilization.
SOURCES: The BMJ, Jan. 21, 2026; Dr. Anne Steiner, president, Society for Reproductive Endocrinology and Infertility





